Home > What’s Happening? > Standards of Care: Who Defines it, How, and Why it Matters
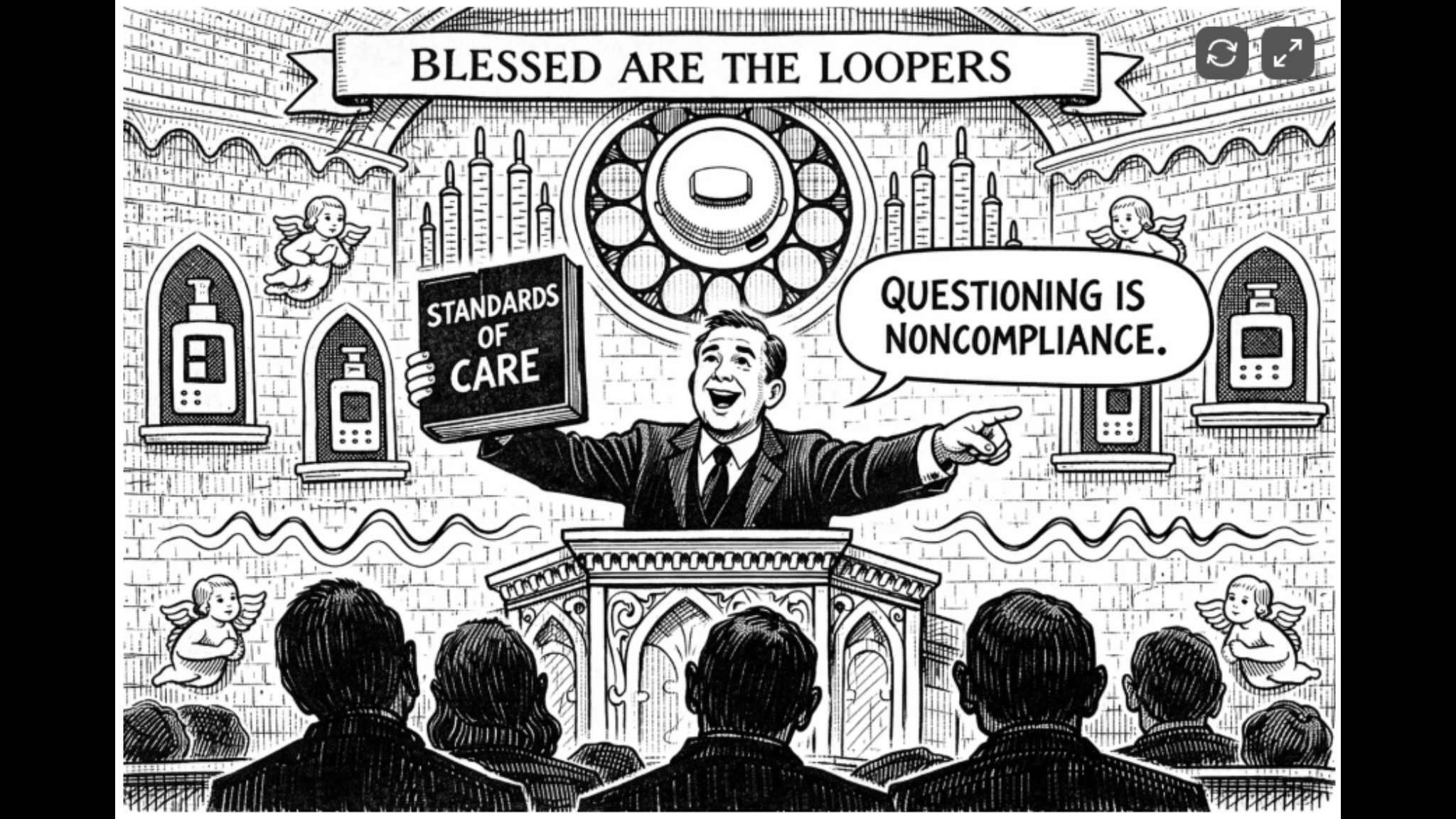
Standards of Care: Who Defines it, How, and Why it Matters
by Dan Heller for DanHeller.substack.com, 24 January 2026. A primer on the ADA’s “recommendations.”
What is the ADA’s Authority? The ADA (founded 1940) is a professional medical association whose members are physicians who pay dues. Those dues-paying members are the intended recipients of the ADA’s communications. The ADA publishes peer-reviewed journals (Diabetes Care, Diabetes, Clinical Diabetes, and hers) and has established credentialing within the broader medical establishment. The ADA’s primary function, as it were, is to develop public policy that its members can use broadly and generally to address the entire population of people with various forms of diabetes. The ADA derives its influence from a combination of factors rather than any legal charter:
- Professional legitimacy
- Institutional adoption: The real power comes from downstream adoption.
- Payer alignment
- The target audience is health care providers (HCPs), who are dues-paying members of the ADA and most of whom are either not trained in diabetes management, or (even if they are) don’t have the time and/or experience to give focused, dedicated attention to individuals, due to their overload of patients.
According to a report by The American Diabetes Association, “the vast majority of individuals with diabetes receive care in primary care settings—not endocrinologists.” In America, the number of endocrinologists is at an all-time low and dropping fast, as medical students are not entering the field. Of those endocrinologists who do treat diabetes, the overwhelming majority treat Type 2 diabetes, which represents approximately 91% of all diabetes cases versus just 6% for Type 1. Given that T2D prevalence is roughly 20-25 times that of T1D, this leaves perhaps 15-25% of endocrinologists with meaningful T1D caseloads.
Put it all together: It’s a reasonable inference that only 5-10% of all endocrinologists are truly proficient in modern T1D management (AID systems, CGM interpretation, exercise physiology, carb-ratio optimization). With 2.1 million T1Ds in the US, chances are pretty high that your doctor is not in that 5-10% of endos that are truly experienced in T1D management.
Nothing in medicine is universally beneficial, and there are often hotly debated topics that are left unresolved. The takeaway is that “standard of care” is a phrase that deserves scrutiny, not reflexive acceptance. Who’s saying it? Based on what evidence? With what accountability? And—perhaps most importantly—does it apply to you? The best defense against borrowed authority is informed skepticism. Understand the difference between advocacy and clinical recommendation guidelines. Read the primary sources.
To read the complete article: https://danheller.substack.com/p/standard-of-care-primer
Recent Stories & News
When the Doctor Needs a Checkup
Taking Control of Your Diabetes (TCOYD) hosts Dr. Steve Edelman and Dr. Jeremy Pettus sit down with endocrinologist Dr. Jennie Luna to discuss inflammation and diabetes.
TCOYD Podcast Ep 92: Inflammation and Diabetes with Dr. Jennie Luna
Taking Control of Your Diabetes (TCOYD) hosts Dr. Steve Edelman and Dr. Jeremy Pettus sit down with endocrinologist Dr. Jennie Luna to discuss inflammation and diabetes.

How to Spot the Subtle Thinking Patterns That Can Accelerate Dementia
A recent study suggests that constant, repetitive patterns of negative thinking, a ‘fatalistic attitude’, could lead to earlier onset or amplified symptoms of dementia. In short, constant negative thinking could cause or amplify dementia.

LGBTQ+ Webinar
For more information about issues facing LGBTQ+ older adults, please check out the Justice in Aging upcoming webinar with SAGE and Lambda Legal.
Aging with T1D: There’s Always Something to Laugh About
Brad Slaight is a comedian, actor, writer, producer, filmmaker, and all-around fun and funny guy. He’s also a T1D – creator of the Diabetes Hero Squad – who’s known for bringing a few laughs to our complicated lives. We sat down with Brad to find out more about what he’s up to and see what he has to say about aging with T1D.
0 Comments